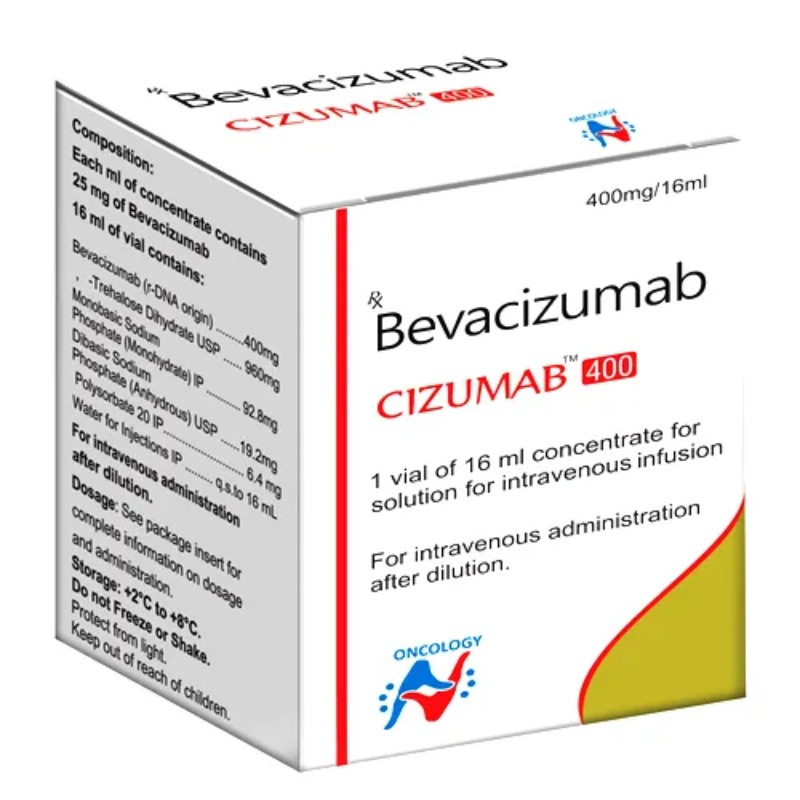
DESCRIPTION
Mechanism of Action
• Recombinant humanized monoclonal antibody directed against the
vascular endothelial growth factor (VEGF). Binds to all isoforms of
VEGF-A. VEGF is a pro-angiogenic growth factor that is overexpressed
in a wide range of solid human cancers, including colorectal cancer.
• Precise mechanism(s) of action remains unknown.
• Binding of VEGF prevents its subsequent interaction with VEGFRreceptors
on the surface of endothelial cells and tumors, and in so
doing, results in inhibition of VEGFR-signaling.
• Inhibits formation of new blood vessels in primary tumor and
metastatic tumors.
• Inhibits tumor blood vessel permeability and reduces interstitial
tumoral pressures, and in so doing, may enhance blood flow delivery
within tumor.
• Restores antitumor response by enhancing dendritic cell function.
• Immunologic mechanisms may also be involved in antitumor
activity, and they include recruitment of ADCC and/or complementmediated
cell lysis.
Mechanism of Resistance
• Increased expression of pro-angiogenic factor ligands, such as PlGF,
bFGF, and hepatocyte growth factor (HGF).
• Recruitment of bone marrow–derived cells, which circumvents the
requirement of VEGF signaling and restores neovascularization and
tumor angiogenesis.
• Increased pericyte coverage of the tumor vasculature, which serves to
support its integrity and reduces the need for VEGF-mediated
survival signaling.
• Activation and enhancement of invasion and metastasis to provide
access to normal tissue vasculature without obligate neovascularization.
Distribution
Distribution in body is not well characterized. The predicted time to reach
steady-state levels is on the order of 100 days.
Metabolism
Metabolism of bevacizumab has not been extensively characterized.
Peripheral half-life is on the order of 17–21 days with minimal clearance by
the liver or kidneys. Tissue half-life has not been well-characterized.
Indications
1. Metastatic colorectal cancer—FDA-approved for use in combination
with any intravenous 5-fluorouracil (5-FU)–based chemotherapy in
first-line therapy.
2. Metastatic colorectal cancer—FDA-approved for use in the second-line
setting in combination with fluoropyrimidine-based chemotherapy
after progression on first-line treatment that includes bevacizumab.
3. Non–small cell lung cancer—FDA-approved for nonsquamous,
NSCLC in combination with carboplatin/paclitaxel.
4. Glioblastoma—FDA-approved as a single agent for glioblastoma with
progressive disease following prior therapy.
5. Renal cell cancer—FDA-approved in combination with interferon-α
for metastatic renal cell cancer.
6. Cervical cancer—FDA-approved in combination with cisplatin/
paclitaxel or paclitaxel/topotecan for metastatic or recurrent cervical
cancer.
Dosage Range
1. Recommended dose for the first-line treatment of advanced colorectal
cancer is 5 mg/kg IV in combination with intravenous
5-FU–based chemotherapy on an every 2-week schedule.
2. Recommended dose for the second-line treatment of advanced
colorectal cancer in combination with FOLFOX-4 is 10 mg/kg IV on
an every 2-week schedule.
3. Can also be administered at 7.5 mg/kg IV every 3 weeks when used
in combination with capecitabine-based regimens for advanced
colorectal cancer.
4. Recommended dose for advanced NSCLC is 15€mg/kg IV every
3 weeks with carboplatin/paclitaxel.
5. Recommended dose for glioblastoma is 10 mg/kg IV every 2 weeks.
Chemotherapeutic and Biologic Drugs 51
B 6. Recommended dose for renal cell cancer is 10 mg/kg IV every
2€weeks with interferon-α.
7. Recommended dose for cervical cancer is 15 mg/kg every 3 weeks
with cisplatin/paclitaxel or paclitaxel/topotecan.
Drug Interactions
None well characterized to date.
Special Considerations
1. Patients should be warned of the increased risk of arterial
thromboembolic events, including myocardial infarction and stroke.
Risk factors are age $65 years and history of angina, stroke, and
prior arterial thromboembolic events. This represents a black-box
warning.
2. Patients should be warned of the potential for serious and, in some
cases, fatal hemorrhage resulting from hemoptysis in patients with
NSCLC. These events have been mainly observed in patients with a
central, cavitary, and/or necrotic lesion involving the pulmonary vasculature
and have occurred suddenly. Patients with recent hemoptysis
($1/2 tsp of red blood) should not receive bevacizumab. This represents
a black-box warning.
3. Bevacizumab treatment can result in the development of GI perforations,
which in some cases has resulted in death. This event represents
a black-box warning for the drug. Use with caution in patients
who have undergone recent surgical and/or invasive procedures.
Bevacizumab should be given at least 28 days after any surgical and/
or invasive intervention.
4. Bevacizumab treatment can result in the development of wound
dehiscence, which in some cases can be fatal. This represents a
black-box warning. Use with caution in patients who have undergone
recent surgical and/or invasive procedures. Bevacizumab should be
given at least 28 days after any surgical and/or invasive intervention.
5. Carefully monitor for infusion-related symptoms. May need to treat
with diphenhydramine (Benadryl) and acetaminophen.
6. Use with caution in patients with uncontrolled hypertension as bevacizumab
can result in grade 3 hypertension in about 10% of patients.
Should be permanently discontinued in patients who develop hypertensive
crisis. In most cases, however, hypertension is well-managed
by increasing the dose of the antihypertensive medication and/or
with the addition of another antihypertensive medication.
7. Bevacizumab should be terminated in patients who develop the
nephrotic syndrome. Therapy should be interrupted for proteinuria
$2 grams/24 hours and resumed when ,2 grams/24 hours.
B 8. Bevacizumab treatment can result in reversible posterior leukoencephalopathy
syndrome (RPLS), as manifested by headache, seizure,
lethargy, confusion, blindness and other visual side effects, as well as
other neurologic disturbances. This syndrome can occur from
16€hours to 1 year after initiation of therapy, and usually resolves or
improves within days, and magnetic resonance imaging is necessary
to confirm the diagnosis.
9. There are no recommended dose reductions for bevacizumab. In the
setting of adverse events, bevacizumab should be discontinued or
temporarily interrupted.
10. Pregnancy category B.
Toxicity 1
Gastrointestinal perforations and wound-healing complications.
Toxicity 2
Bleeding complications with epistaxis being most commonly observed.
Serious, life-threatening pulmonary hemorrhage occurs in rare cases in
patients with NSCLC, as outlined previously in Special Considerations.
Toxicity 3
Increased risk of arterial thromboembolic events, including myocardial
infarction, angina, and stroke. There is also an increased incidence of venous
thromboembolic events.
Toxicity 4
Hypertension occurs in 5–18%. Usually well controlled with oral antihypertensive
medication.
Toxicity 5
Proteinuria with nephrotic syndrome ,1%.
Toxicity 6
Infusion-related symptoms with fever, chills, urticaria, flushing, fatigue,
headache, bronchospasm, dyspnea, angioedema, and hypotension. Infusion
reactions occur in ,3% of patients and severe reactions occur in 0.2% of
patients.
Toxicity 7
CNS events with dizziness and depression. RPLS occurs rarely (incidence
of ,0.1%) and presents with headache, seizure, lethargy, confusion, blindness,
and other visual disturbances.
SPECIFICATION
Login To Comment