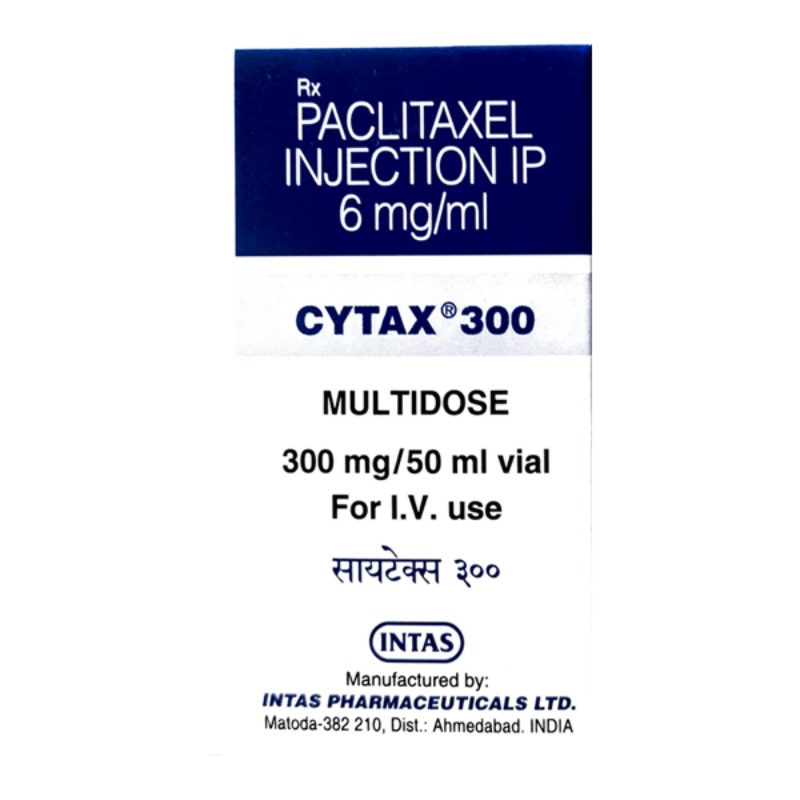
DESCRIPTION
PACLITAXEL
Mechanism of Action
• Isolated from the bark of the Pacific yew tree, Taxus brevifolia.
• Cell cycle–specific, active in the mitosis (M) phase of the cell cycle.
• High-affinity binding to microtubules enhances tubulin polymerization.
Normal dynamic process of microtubule network is inhibited,
leading to inhibition of mitosis and cell division.
Mechanism of Resistance
• Alterations in tubulin with decreased binding affinity for drug.
• Multidrug-resistant phenotype with increased expression of P170
 glycoprotein. Results in enhanced drug efflux with decreased intracellular
accumulation of drug. Cross-resistant to other natural products,
including vinca alkaloids, anthracyclines, taxanes, and VP-16.
Absorption
Poorly soluble and not orally bioavailable.
Distribution
Distributes widely to all body tissues, including third-space fluid collections
such as ascites. Negligible penetration into the CNS. Extensive binding
(.90%) to plasma and cellular proteins.
Metabolism
Metabolized extensively by the hepatic P450 microsomal system. About
70%–80% of drug is excreted via fecal elimination. Less than 10% is eliminated
as the parent form with the majority being eliminated as metabolites.
Renal clearance is relatively minor with less than 10% of drug cleared via the
kidneys. Terminal elimination half-life ranges from 9 to 50 hours depending
on the schedule of administration.
Indications
1. Ovarian cancer.
2. Breast cancer.
3. Non–small cell and small cell lung cancer.
4. Head and neck cancer.
5. Esophageal cancer.
6. Prostate cancer.
7. Bladder cancer.
8. AIDS-related Kaposi’s sarcoma.
Dosage Range
1. Ovarian cancer: 135–175 mg/m2 IV as a 3-hour infusion every
3 weeks.
2. Breast cancer: 175 mg/m2 IV as a 3-hour infusion every 3 weeks.
3. Bladder cancer, head and neck cancer: 250 mg/m2 IV as a 24-hour
infusion every 3 weeks.
4. Weekly schedule: 80–100 mg/m2 IV each week for 3 weeks with
1-week rest.
5. Infusional schedule: 140 mg/m2 as a 96-hour infusion.
Drug Interaction 1
Radiation therapy—Paclitaxel is a radiosensitizing agent.
Drug Interaction 2
Concomitant use of inhibitors and/or activators of the liver P450 CYP3A4
enzyme system may affect paclitaxel metabolism and its subsequent antitumor
and toxic effects.
Drug Interaction 3
Phenytoin, phenobarbital—Accelerate the metabolism of paclitaxel resulting
in lower plasma levels of drug.
Drug Interaction 4
Cisplatin, carboplatin—Myelosuppression is greater when platinum compound
is administered before paclitaxel. Platinum compounds inhibit
plasma clearance of paclitaxel. When a platinum analog is used in combination,
paclitaxel must be given first.
Drug Interaction 5
Cyclophosphamide—Myelosuppression is greater when cyclophosphamide
is administered before paclitaxel.
Drug Interaction 6
Doxorubicin—Paclitaxel reduces the plasma clearance of doxorubicin by
about 30%, resulting in increased severity of myelosuppression.
Special Considerations
1. Contraindicated in patients with history of severe hypersensitivity
reaction to paclitaxel or to other drugs formulated in Cremophor EL,
including cyclosporine, etoposide, or teniposide.
2. Use with caution in patients with abnormal liver function. Dose
reduction is required in this setting. Patients with abnormal liver
function are at significantly higher risk for toxicity. Contraindicated
in patients with severe hepatic dysfunction.
3. Use with caution in patients with prior history of diabetes mellitus
and chronic alcoholism or prior therapy with known neurotoxic
agents such as cisplatin.
4. Use with caution in patients with previous history of ischemic heart
disease, with MI within the preceding 6 months, conduction system
abnormalities, or on medications known to alter cardiac conduction
(beta blockers, calcium channel blockers, and digoxin).
5. Patients should receive premedication to prevent the incidence of
hypersensitivity reactions (HSR). Give dexamethasone 20 mg PO at
12 and 6 hours before drug administration, diphenhydramine 50 mg
IV, and cimetidine 300 mg IV at 30 minutes before drug administration.
Patients experiencing major HSR may be rechallenged after
receiving multiple high doses of steroids, dexamethasone 20 mg IV
every 6 hr for 4 doses. Patients should also be treated with diphenhydramine
50 mg IV and cimetidine 300 mg IV 30 minutes before
the rechallenge.
6. Medical personnel should be readily available at the time of drug
administration. Emergency equipment, including Ambu bag, ECG
machine, IV fluids, pressors, and other drugs for resuscitation,
must be at bedside before initiation of treatment.
7. Monitor patient’s vital signs every 15 minutes during the first hour of
drug administration. HSR usually occurs within 2–3 minutes of start
of infusion and almost always within the first 10 minutes.
8. Patients who have received >6 courses of weekly paclitaxel should be
advised to avoid sun exposure of their skin as well as their fingernails
and toenails, as they are at increased risk for developing onycholysis.
This side effect is not observed with the every 3-week schedule.
9. Pregnancy category D. Breastfeeding should be avoided.
Toxicity 1
Myelosuppression. Dose-limiting neutropenia with nadir at day 8–10 and
recovery by day 15–21. Decreased incidence of neutropenia with 3-hour
schedule when compared to 24-hour schedule.
Toxicity 2
Infusion reactions. Occurs in up to 20%–40% of patients. Characterized
by generalized skin rash, flushing, erythema, hypotension, dyspnea, and/or
bronchospasm. Usually occurs within the first 2–3 minutes of an infusion
and almost always within the first 10 minutes. Incidence of HSR is the same
with 3- and 24-hour schedules. Premedication regimen, as outlined in
Special Considerations, has significantly decreased incidence.
Toxicity 3
Neurotoxicity mainly in the form of sensory neuropathy with numbness
and paresthesias. Dose-dependent effect. Other risk factors include prior
exposure to known neurotoxic agents (e.g., cisplatin) and pre-existing medical
disorders such as diabetes mellitus and chronic alcoholism. More frequent
with longer infusions and at doses .175 mg/m2. Motor and autonomic
neuropathy observed at high doses. Optic nerve disturbances with scintillating
scotomata observed rarely.
Toxicity 4
Transient asymptomatic sinus bradycardia is most commonly observed
cardiotoxicity. Occurs in 30% of patients. Other rhythm disturbances are
seen, including Mobitz type I, Mobitz type II, and third-degree heart block,
as well as ventricular arrhythmias.
Toxicity 5
Alopecia. Occurs in nearly all patients, with loss of total body hair.
Toxicity 6
Mucositis and/or diarrhea seen in 30%–40% of patients. Mucositis is
more common with the 24-hour schedule. Mild-to-moderate nausea and
vomiting, usually of brief duration.
Toxicity 7
Transient elevations in serum transaminases, bilirubin, and alkaline
phosphatase.
Toxicity 8
Onycholysis. Mainly observed in those receiving >6 courses on the weekly
schedule. Not seen with the every 3-week schedule.
SPECIFICATION

Login To Comment