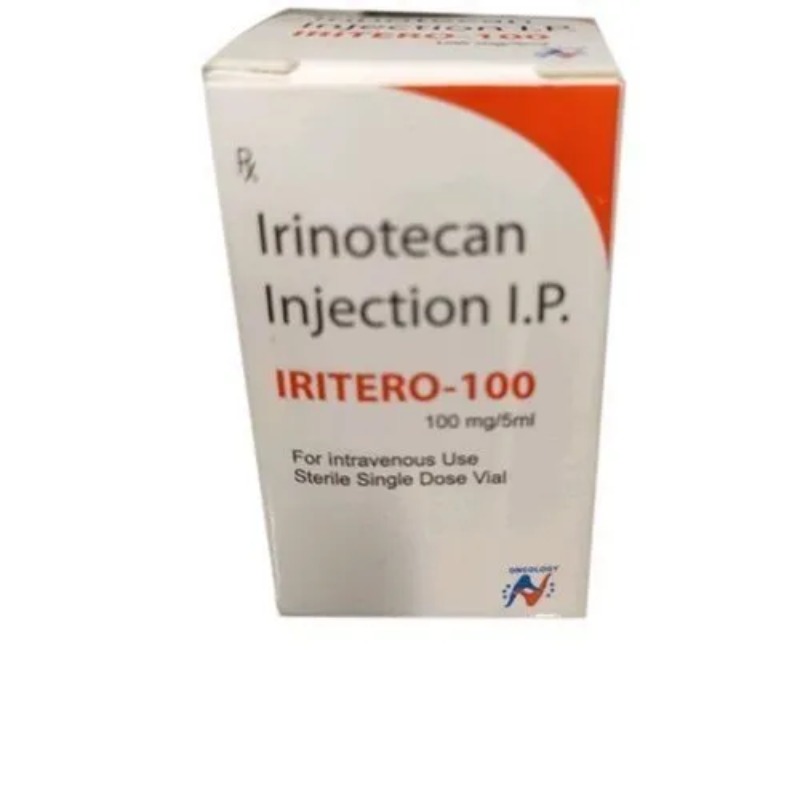
DESCRIPTION
Mechanism of Action
• Semisynthetic derivative of camptothecin, an alkaloid extract from
the Camptotheca acuminata tree.
Chemotherapeutic and Biologic Drugs 263
I • Inactive in its parent form. Converted by the carboxylesterase
enzyme to its active metabolite, SN-38.
• SN-38 binds to and stabilizes the topoisomerase I-DNA complex and
prevents the religation of DNA after it has been cleaved by topoisomerase
I. The collision between this stable, cleavable complex and the
advancing replication fork results in double-strand DNA breaks and
cellular death.
• Antitumor activity of drug requires the presence of ongoing DNA
synthesis.
• Cell cycle–nonspecific agent with activity in all phases of the cell
cycle.
• Colorectal tumors express higher levels of topoisomerase I than normal
colonic mucosa, making this an attractive target for chemotherapy.
Mechanism of Resistance
• Decreased expression of topoisomerase I.
• Mutations in topoisomerase I enzyme with decreased affinity for the
drug.
• Increased expression of the multidrug-resistant phenotype with overexpression
of P170 glycoprotein. Results in enhanced efflux of drug
and decreased intracellular accumulation of drug.
• Decreased formation of the cytotoxic metabolite SN-38 through
decreased activity and/or expression of the carboxylesterase enzyme.
• Decreased accumulation of drug into cells by mechanisms not well
identified.
Absorption
Irinotecan is administered only by the IV route.
Distribution
Widely distributed in body tissues. Irinotecan exhibits moderate binding
to plasma proteins (30%–60%). In contrast, SN-38 shows extensive plasma
protein binding (95%). Peak levels of SN-38 are achieved within 1 hour after
drug administration.
Metabolism
The conversion of irinotecan to the active metabolite SN-38 occurs primarily
in the liver. However, this conversion can also take place in plasma
and in intestinal mucosa. SN-38 subsequently undergoes conjugation in the
liver to the glucuronide metabolite, which is essentially inactive. In aqueous
solution, the lactone ring undergoes rapid hydrolysis to the carboxylate form.
Only about 34%–44% of CPT-11 and 45%–64% of the active metabolite
SN-38 are present in the active lactone form at 1 hour after drug administra
I tion. The major route of elimination of both irinotecan and SN-38 is in bile
and feces, accounting for 50%–70% of drug clearance. Only 10%–14% of
CPT-11 and ,1% of SN-38 is cleared in urine. The half-lives of irinotecan and
SN-38 are 6–12 and 10–20 hours, respectively.
Indications
1. Colorectal cancer—FDA-approved in combination with 5-FU and leucovorin
as first-line treatment of patients with metastatic colorectal cancer.
2. Colorectal cancer—FDA-approved as a single agent for second-line
treatment of patients with metastatic colorectal cancer after failure of
5-FU–based chemotherapy.
3. Non–small cell lung cancer.
4. Small cell lung cancer.
Dosage Range
1. Irinotecan can be administered at 180 mg/m2 IV as monotherapy or
in combination with infusional 5-FU/LV on an every-2-week schedule.
2. An alternative regimen is 300–350 mg/m2 IV on an every-3-week
schedule.
Drug Interaction 1
Phenytoin and other drugs that stimulate the liver microsomal CYP3A4
enzyme, including carbamazepine, rifampin, phenobarbital, and St. John’s
Wort—These drugs increase the rate of metabolism of irinotecan and SN-38,
resulting in its inactivation.
Drug Interaction 2
Drugs that inhibit the liver microsomal CYP3A4 enzymes, including
ketoconazole, itraconazole, erythromycin, and clarithromycin—These drugs
decrease the rate of metabolism of irinotecan and SN-38, resulting in
increased drug levels and potentially increased toxicity.
Special Considerations
1. Irinotecan is an emetogenic drug. Patients should routinely receive
antiemetic prophylaxis with a 5-HT3 antagonist, such as ondansetron
or granisetron, in combination with dexamethasone.
2. Treatment with irinotecan is complicated by a syndrome of “early
diarrhea,” which consists of diarrhea, diaphoresis, and abdominal
cramping during the infusion or within 24 hours of drug administration.
This complication is thought to be due to a cholinergic effect.
The recommended treatment is atropine (0.25–1.0 mg) administered
IV unless clinically contraindicated. The routine use of atropine for
prophylaxis is not recommended. However, atropine prophylaxis
should be administered if a cholinergic event has been experienced.
3. Instruct patients about the possibility of late diarrhea (starting after
24 hours of drug administration), which can lead to serious dehydration
and/or electrolyte imbalances if not managed promptly. This
side effect is thought to be due to a direct irritation of the gastrointestinal
mucosa by SN-38, although other as yet unidentified mechanisms
may be involved. Loperamide should be taken immediately
after the first loose bowel movement. The recommended dose is
4 mg PO as a loading dose, followed by 2 mg every 2 hours around
the clock (4 mg every 4 hours during the night). Loperamide can be
discontinued once the patient is diarrhea-free for 12 hours. If diarrhea
should continue without improvement in the first 24 hours, an
oral fluoroquinolone should be added. Hospitalization with IV antibiotics
and IV hydration should be considered with continued diarrhea.
4. Irinotecan should be held for grade 3 (7–9 stools/day, incontinence,
or severe cramping) and/or grade 4 (<10 stools/day, grossly bloody
stool, or need for parenteral support) diarrhea. Dose of drug must be
reduced upon recovery by the patient.
5. Patients should be warned against taking laxatives while on therapy.
6. Carefully monitor administration of drug as it is a moderate vesicant.
The site of infusion should be carefully inspected for extravasation,
in which case flushing with sterile water, elevation of the extremity,
and local application of ice are recommended.
7. Use with caution in patients >65 years of age, in patients with poor
performance status, and in those previously treated with pelvic and/
or abdominal irradiation as they are at increased risk for myelosuppression
and diarrhea.
8. Careful monitoring of patients on a weekly basis, especially during
the first treatment cycle. Monitor complete blood cell count and
platelet count on a weekly basis.
9. Patients with the UGT1A1 7/7 genotype may be at increased risk for
developing GI toxicity and myelosuppression. Approximately 10% of
the North American population is homozygous for this genotype.
Dose reduction should be considered in this setting.
10. Patients should be warned to be off St. John’s Wort for at least 2 weeks
before starting irinotecan therapy and should remain off until after
the completion of irinotecan therapy. St. John’s Wort has been shown
to reduce the efficacy of irinotecan chemotherapy by inhibiting
metabolism of irinotecan to the active SN-38 metabolite.
11. Pregnancy category D. Breastfeeding should be avoided.
Toxicity 1
Myelosuppression. Dose-limiting with neutropenia being most commonly
observed. Patients with prior history of abdominal/pelvic irradiation
I are particularly prone to developing myelosuppression after treatment with
irinotecan. Typical nadir occurs at days 7–10 with full recovery by days 21–28.
Toxicity 2
Diarrhea. Dose-limiting with two different forms, early and late. Early
form occurs within 24 hours of drug treatment and is thought to be a cholinergic
event. Characterized by flushing, diaphoresis, abdominal pain, and
diarrhea. Late-form diarrhea occurs after 24 hours, typically at 3–10 days after
treatment, can be severe and prolonged, and can lead to dehydration and
electrolyte imbalance. Up to 80%–90% of patients may experience some
aspect of late diarrhea, although only 10%–20% of patients will experience
grade 3 or 4 diarrhea. Anorexia, nausea, and vomiting are usually mild and
dose-related.
Toxicity 3
Mild alopecia.
Toxicity 4
Transient elevation in serum transaminases, alkaline phosphatase, and
bilirubin.
Toxicity 5
Asthenia and fever.
SPECIFICATION
Login To Comment