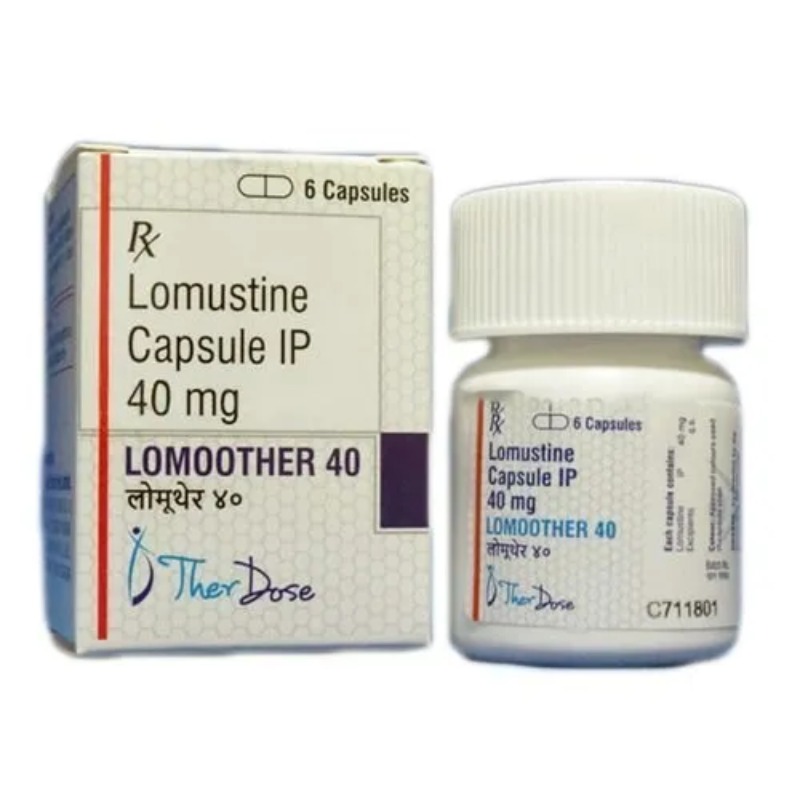
DESCRIPTION
Mechanism of Action
• Cell cycle–nonspecific nitrosourea analog.
• Alkylation and carbamoylation by lomustine metabolites interfere
with the synthesis and function of DNA, RNA, and proteins.
• Antitumor activity appears to correlate best with formation of intrastrand
cross-linking of DNA.
Mechanism of Resistance
• Decreased cellular uptake of drug.
• Increased intracellular thiol content due to glutathione and/or
glutathione-related enzymes.
• Enhanced activity of DNA repair enzymes.
Absorption
Readily and completely absorbed orally. Peak plasma concentrations are
observed within 3 hours after oral administration.
Distribution
Lipid-soluble drug with broad tissue distribution. Well-absorbed after oral
administration and crosses the blood-brain barrier. CNS levels approach
15%–30% of plasma levels.
Metabolism
Metabolized by the liver microsomal P450 system to active metabolites.
The elimination half-life of the drug is about 72 hours, and excretion mainly
occurs via the kidneys. Approximately 50% of a dose is excreted in urine within
the first 12–24 hours, while 60% of a dose is excreted after 48 hours.
Indications
1. Brain tumors—Early-stage or metastatic.
2. Hodgkin’s lymphoma.
3. Non-Hodgkin’s lymphoma.
Dosage Range
Recommended dose as a single agent in previously untreated patients is
130 mg/m2 PO every 6 weeks. In patients with compromised bone marrow
function, the dose should be reduced to 100 mg/m2 PO every 6 weeks.
Drug Interaction 1
Cimetidine—Cimetidine enhances the toxicity of lomustine.
Drug Interaction 2
Alcohol—Ingestion of alcohol should be avoided for at least 1 hour before
and after administration of lomustine.
Special Considerations
1. Monitor CBC while on therapy. Subsequent cycles should not be
given before 6 weeks, given the delayed and potentially cumulative
effects of the drug. Platelet and leukocyte counts must return to
normal before starting the next course of therapy.
2. PFTs should be obtained at baseline and monitored periodically
during therapy. There is an increased risk of pulmonary toxicity in
patients with a prior history of lung disease and a baseline FVC or
DLCO below 70% of predicted.
3. Administer drug on an empty stomach as food may inhibit
absorption.
4. Pregnancy category D. Breastfeeding should be avoided.
Toxicity 1
Myelosuppression is dose-limiting. In contrast to most other anticancer
agents, myelosuppression involving all elements is delayed and cumulative.
Nadirs typically occur 4–6 weeks after therapy and may persist for 1–3 weeks.
Toxicity 2
Nausea and vomiting may occur within 2–6 hours after a dose of drug
and can last for up to 24 hours.
Toxicity 3
Anorexia may be present but short-lived. Mucositis is unusual.
Toxicity 4
Impotence, male sterility, amenorrhea, ovarian suppression, menopause,
and infertility. Gynecomastia is occasionally observed.
Toxicity 5
Pulmonary toxicity is uncommon at doses lower than 1100 mg/m2.
Toxicity 6
Interstitial lung disease and pulmonary fibrosis in the form of an insidious
cough, dyspnea, pulmonary infiltrates, and/or respiratory failure may be
observed.
Toxicity 7
Renal toxicity is uncommon at total cumulative doses of lower than
1000 mg/m2. Usually manifested by progressive azotemia and decrease in
kidney size, which can progress to renal failure.
Toxicity 8
Neurotoxicity in the form of confusion, lethargy, dysarthria, and ataxia.
Toxicity 9
Increased risk of secondary malignancies with long-term use, especially
acute myelogenous leukemia and myelodysplasia.
Toxicity 10
Alopecia is rarely seen.
SPECIFICATION
Login To Comment